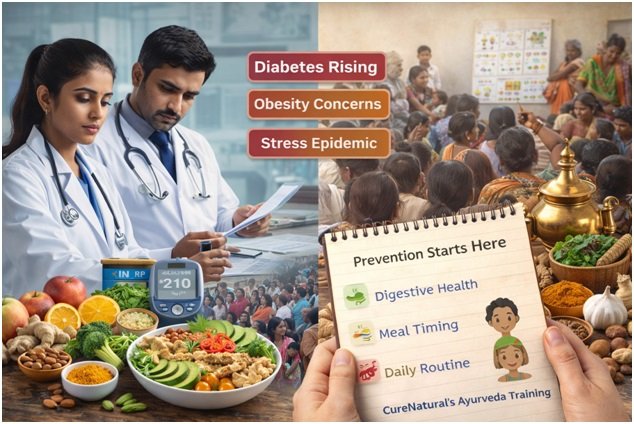
India is facing a silent epidemic. Lifestyle-related diseases such as diabetes, hypertension, digestive disorders, obesity, and stress-related conditions are rising rapidly across both urban and rural populations. What makes this crisis particularly challenging is not just treatment cost, but sustainability.
Healthcare systems are increasingly reactive. They intervene once disease is established, often too late and at great expense. What is missing is a scalable, preventive framework that empowers individuals long before chronic illness sets in.
This is where traditional health systems, when applied thoughtfully, may offer a meaningful solution.
The Growing Cost of Lifestyle Disease
India now accounts for one of the largest populations living with diabetes and cardiovascular disease globally. These conditions are driven not by infectious agents, but by daily habits—food choices, meal timing, stress, sleep, and physical activity.
The economic impact is substantial. Long-term medication use, hospitalizations, productivity loss, and caregiver burden place strain on families and public systems alike. Yet many of these conditions are preventable or reversible in early stages.
Prevention, however, requires more than awareness campaigns. It requires practical, culturally aligned education that people can apply in daily life.
Why Prevention Often Fails in Practice
Most public health messaging focuses on generic advice: eat healthy, exercise more, reduce stress. While well-intentioned, such guidance lacks specificity. People struggle to translate it into action because it does not account for individual differences in digestion, metabolism, work schedules, or climate.
A one-size-fits-all approach is easy to communicate but difficult to implement. As a result, compliance is low and outcomes are inconsistent.
Effective prevention must meet people where they are—culturally, biologically, and socially.
Ayurveda as a Preventive Framework
Ayurveda, one of India’s traditional systems of health, was designed primarily as a preventive science. Rather than focusing on disease labels, it emphasizes balance in digestion, metabolism, daily routine, and mental state.
Individuals are understood to differ in digestive strength, energy patterns, and stress response. Food, lifestyle, and daily timing are adjusted accordingly. This personalization is not cosmetic. It is central to the system’s logic.
What makes Ayurveda relevant today is not nostalgia, but structure. Its principles offer a way to categorize risk early, long before laboratory values cross pathological thresholds.
Aligning Tradition With Modern Public Health
For traditional systems to contribute meaningfully to modern healthcare, they must be applied responsibly. This means education over dogma, and prevention over promise.
Programs such as Cure Natural’s Ayurveda training focus on teaching individuals how to recognize early imbalances, improve digestion with Ayurveda, align meals with natural rhythms, and reduce stress through practical routines. The emphasis is on self-care literacy, not dependency.
When individuals understand why certain foods or habits affect them negatively, behavior change becomes sustainable rather than forced.
Community-Level Impact and Scalability
One of the strengths of traditional preventive systems is scalability. Education can be delivered through community programs, schools, workplaces, and digital platforms. The cost per individual is low compared to long-term treatment.
CSR initiatives that integrate preventive education can reduce absenteeism, improve workforce well-being, and lower healthcare utilization over time. For underserved populations, early education may prevent decades of chronic illness.
Importantly, such approaches do not replace modern medicine. They complement it by reducing the load on tertiary care.
The Role of Cultural Familiarity
Health advice resonates more strongly when it aligns with cultural context. Ayurveda is not foreign to Indian households. Its language around food, routine, and balance is already embedded in daily life, even if applied inconsistently.
By modernizing delivery while respecting tradition, preventive education becomes more accessible and less intimidating. This increases trust and engagement—critical components of public health success.
A Shift From Treatment to Resilience
The future of healthcare in India cannot rely solely on expanding hospitals and pharmaceutical access. It must also invest in resilience-building—helping people maintain health rather than manage disease.
Traditional systems, when integrated thoughtfully and taught responsibly, can play a role in this shift. They offer a framework for early intervention, personalization, and daily self-regulation.
The question is no longer whether India can afford to invest in prevention. It is whether it can afford not to.